How We Approach Your Care
You get more than just treatment - you get a true partnership in your recovery.
Rather than simply masking symptoms, we take the time to understand exactly what's happening with your feet and lower limbs. You'll experience cutting-edge techniques combined with genuine care, all tailored specifically to your situation and life stage.
Your journey follows a structured process designed around your needs.
Whether you're in pain right now, working through an injury, or wanting to perform at your best, you'll have expert guidance at every step. From your first consultation through to achieving your goals, you'll know exactly what's happening and why - because your understanding and comfort matter as much as your results.
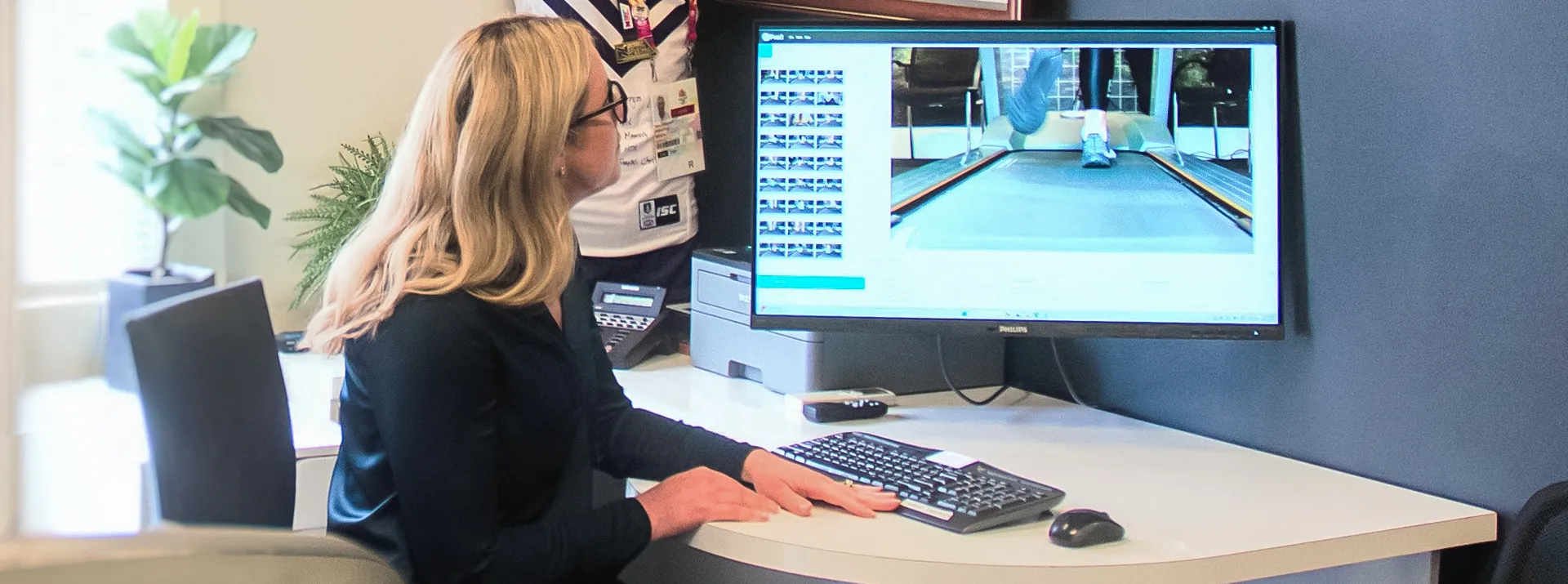
Comprehensive Assessment
We start with a thorough evaluation of your feet, lower limbs, and biomechanics to pinpoint the root cause of your concerns. This evaluation is not just static, but extensive dynamic assessment with state of the art equipment and facilities not seen in other clinics.
Tailored treatment plan
Based on your assessment, we create a personalised care plan using the latest in podiatric technology and evidence-based techniques.
Ongoing Support and Education
We empower you with the tools, exercises, and insights needed to manage and prevent future issues, ensuring lasting results.
Preventive Care and Optimisation
Whether you’re an athlete, a parent, or managing chronic conditions, we work with you to optimise performance and maintain peak health
Comprehensive Assessment
We start with a thorough evaluation of your feet, lower limbs, and biomechanics to pinpoint the root cause of your concerns. This evaluation is not just static, but expensive dynamic assessment with state of the art equipment and facilities not seen in other clinics.
Tailored treatment plan
Based on your assessment, we create a personalised care plan using the latest in podiatric technology and evidence-based techniques.
Ongoing Support and Education
We empower you with the tools, exercises, and insights needed to manage and prevent future issues, ensuring lasting results.
Preventive Care and Optimisation
Whether you’re an athlete, a parent, or managing chronic conditions, we work with you to optimise performance and maintain peak health
Conditions We Treat
Our team provides expert care for a wide range of foot and lower limb issues, including:
Foot & Ankle

Plantar Fasciitis



Plantar Fasciitis
This is the most common cause of all heel pains. The plantar fascia is a band of fibrous connective tissue that runs along the sole from the heel to the ball of the foot. Bruising or over stretching this can cause inflammation particularly more towards the heel but can affect any part of the band.
It is commonly associated with long periods of weight bearing or sudden changes in activity levels Prevention and treatment will often revolve around stretching, massage, change of footwear and possibly orthotics if there is an underlying biomechanical cause.


Flat Feet



Flat Feet
Have you ever been told, or have you always been aware that your feet are flat?
Flat feet are the postural deformity in which the arches of the foot collapse, with the entire sole of the foot coming into complete or near-complete contact with the ground. In many cases these may be asymptomatic, but flat feet are often an indication that the architecture and integrity is not correct. Your feet support the whole body, and having strong arches is important to your body’s health. With a fallen arch, your tendons and ligaments weaken and can cause pain throughout your feet, ankles, lower legs and even further up through to your hips and lower back.
Treatment will often revolve around creating stability. This can be done wearing comfortable and supportive footwear. Wearing the appropriate orthotics can also help distribute and minimise pressure in the foot by providing the additional arch support. Strength and stabilising exercises can also be incorporated for extra control.
It's also important to know that not all flat feet need support. We are here to make sure that options are discussed and expert opinion is provided where treatment IS NOT required where assistance may help. Not all flat feet need orthoses.


Ankle Pain



Ankle Pain
Are you getting ankle pain? You may have an obvious reason for this, like a recent sprain! However sometimes there is a not so obvious reason.
Either way it is important to have it checked out by a qualified Sports Podiatrist. The ankle is an important weight bearing joint. It can be affected by arthritis, ligament injury, fractures and various other pathologies. A thorough assessment is essential for a correct diagnosis so that the right treatment choice can be provided for you.
We aim to give you the best professional advice and care possible here at Peak Podiatry.


Morton's Neuroma



Morton's Neuroma
Are you experiencing a dull ache in your forefoot that sometimes turns into a sharp radiating pain into your toes? Or do you get unexplained numbness at the end of a toe/toes?
These are common symptoms that occur in a condition called Morton’s neuroma. The Morton’s Neuroma is simply described as a thickening of the nerve or surrounding tissue as it passes through the space between the Metatarsal heads. It is usually found between the 3rd and 4th metatarsals but it can occur between the others.
Compression of the forefoot from wearing shoes that are too tight is a common cause. However, there are other biomechanical causes of the pathology that always need to be assessed. In severe cases surgery may be required.


Metatarsal Stress Fractures



Metatarsal Stress Fractures
Stress fractures refer to a tiny “crack” in a bone caused by repetitive stress or force, often from overuse. Approximately 10% of all stress fractures are localised to the metatarsal bones of the foot. Football, basketball, gymnastics, ballet and running are often associated with metatarsal stress fractures.
Symptoms include Insidious onset of pain, frequently worsened with activity with no recollection of trauma or trauma which is 1-2 week(s) prior symptoms. Although x-rays are often utilised in the diagnosis of stress fractures, clinical examinations alone are usually reliable in making the diagnosis.
Footwear modification, activity modification, carbon plates and/or specialised boots are all examples of the immediate treatment available. In the long-term, we can also provide biomechanical assessments to determine if an underlying biomechanical dysfunction is predisposing to the stress fracture and prevent reoccurrence.


Rolled Ankles



Rolled Ankles
This is a very common injury occurring during a wide variety of sports and activities. Usually the ankle “rolls-in” and ligaments and tendons on the outside become aggravated, damaged and sometimes torn depending on the severity of the injury.
The most commonly injured structure is the Anterior Talofibular Ligament (ATFL), which connects the talus to the fibula on the outside of the ankle. It is important to rest, ice, apply compression and elevate the ankle immediately and up-to 48 hours after injury to help with swelling.
If pain persists 48 hours after injury it is always a good idea to see one of our Podiatrists to assess the extent of injury. This is critical as the most important aspect of any ankle injury is setting-up an appropriate rest and rehab protocol. The chances of rolling the same ankle again are significantly higher without appropriate rest and rehab.


Cuboid Syndrome



Cuboid Syndrome
Do you have lateral foot pain (outer side of your foot) that either aches or feels like the pain moves around? Sometimes even feels slightly locked up?
The Cuboid is an important bone in the lateral arch of the foot that can subtly ‘sublux’ when enough force is applied by a tendon that travels over it called the Peroneus Longus This can occur as a one off “incident”, like a slight sprain of the ankle, or gradual tightening of the Peroneus Longus caused by overuse.
While cuboid syndrome is relatively common it is hard to identify so is commonly misdiagnosed. It is important to get it treated early so as to “reposition” the cuboid back into its original place. There can be long term effects on the calcaneocuboid joint and surrounding structures if left in a ‘subluxed’ position for too long.
Biomechanics can play a large part in the foot type that sustains this injury so it is important to always have it assessed by a Podiatrist.

Arthritic Toe Joint Pain

Forefoot Pain



Forefoot Pain
The forefoot (or ball of the foot) is made up of small bones, muscles, ligaments, tendons and many other forms of soft tissues. This makes pain in this area complex to diagnose. An expert knowledge of the anatomy of the forefoot allows an in-depth examination and the injured structure can be easily identified. Often the diagnosis can be as diverse a painful corn or callus to an entrapped nerve.
Management is directed towards targeting the cause and condition, and measures put in place to offload the affected area. These may include a change of footwear or modifications and possibly shoes orthoses. Massage and other forms of remedial therapy can always help.


Bunions and Big Toe Joint Pain



Bunions and Big Toe Joint Pain
Are you starting to notice a lump or bump on the side of your big toe?
Are you experiencing pain in this joint when you are wearing shoes?
Bunions are extremely common conditions seen by Podiatrists. They are often seen as a bony lump near the base of the big toe joint which can eventually lead to osteoarthritis. The first toe joint plays an extremely important role in how we function during walking and running, and changes to this joint can reflect further than the foot itself.
A conservative approach is usually the first line of treatment, all depending on the individual and stage of the deformity. Re-aligning the foot with the aid of an orthotic can prevent further degeneration. Along with this, a change of footwear may help decrease the pressure and compliment the orthotics. Surgical correction of the bunion is another option but should only be considered if the conservative measures have failed.

Leg Pain

Shin Pain



Shin Pain
This is a common injury in many running based sports. It is characterised by pain in and around the tibia (shin bone) in the lower leg and usually occurs as a result of a sudden increase in the frequency, duration and/or intensity of activity.
People at risk are those with abnormal biomechanics, using inappropriate footwear for the activity and often poor flexibility. Prevention initially starts with undertaking adequate and supervised training.
Programmes may be required to develop strength, balance, coordination and flexibility. Wearing the appropriate footwear for your foot type and considering a biomechanical foot screening to determine if further orthomechanical control is required.
Like most overuse injuries, shin pain may develop gradually over a period of time but if assessed and treated early, a return to normal activity levels can be easily achieved.


Calf Strain



Calf Strain
This is a condition caused by a tear of the muscle fibres of the muscles at the back of the lower leg and can range from mild to very severe. Calf injuries usually occur as a result of a sudden pushing off movement or from excessive over-stretching of the calf muscles as demonstrated in jumping activities or during quick changes of direction.
Treatment can include rest, ice, and compression in the acute stages followed by a full rehabilitation programme of strength and stretching exercises. Often Podiatrists will analyse a person’s gait and footwear to ascertain if control is adequate to also prevent further injury.


Foot & Leg Cramps



Foot & Leg Cramps
A muscle cramp is a strong, painful contraction or tightening of a muscle that typically comes on suddenly and can last anywhere from a few seconds to several minutes. It often occurs in the legs and through the calf muscles. However, sometimes it occurs in the small intrinsic foot muscles and is misdiagnosed.
Specific stretching, taping, dry needling and massage techniques can make a massive difference and rid you of any symptoms. Sometimes the cramps are secondary to poor lower limb biomechanics and that can be augmented with footwear modifications or orthotic therapy.

Knee Pain

Patellafemoral



Patellafemoral
This refers to pain arising from under and around the kneecap. The kneecap is designed to move up and down within a special groove at the end of the thigh bone. If the kneecap starts to track to the side (misaligned), pain develops.
With this repeated movement the cartilage behind the kneecap can also become irritated. The most common symptom experienced is pain worsening with running and also going up and down stairs. Common causes can be poor foot mechanics, improper footwear and weakness or an imbalance of the quadriceps muscles.
Treatment will include an adequate gait assessment and review of shoes. Together with strengthening of the affected musculatures, orthotic therapy is often needed to improve foot biomechanics and is effective in resolving pain.


Knee Pain



Knee Pain
Knee pain is a common problem with many causes, ranging from acute injuries, various medical conditions and overuse. It can be localised to a specific area of the knee or be diffuse throughout the knee. Most knee conditions are often accompanied by physical restriction and a thorough physical examination will usually establish the diagnosis.
Common types of knee pain seen by Podiatrists include:
- Patellofemoral pain
- Iliotibial Band Friction Syndrome
- Ligament injuries
- Osteoarthritis
Podiatrists are primary health care providers of the feet and lower limb and commonly treat conditions like these.


Knee Arthritis



Knee Arthritis
Osteoarthritis (OA) is the most common form of knee arthritis which is a degenerative joint disease that can gradually wear down the cartilage in the joint. This results in severe pain and stiffness in the joint. OA can affect both sides of the knee but the most common side affected is the inner (medial) side. Common causes of knee arthritis can range from previous trauma to the area, poor biomechanics of the feet, obesity and genetics.
Treatments often revolve around reducing the impact aggravating the condition. Strengthening exercises are often advised but customised orthotics have been shown to help reduce symptoms.

Children's Foot Development
Solutions for flat feet, gait abnormalities, and growth-related concerns.

Sever's Disease



Sever's Disease
Looking at a child limping off the ground and complaining about pain in their heels is never pleasant.
Sever's disease is the most common cause of heel pain particularly in the young and physically active child. Just before puberty the calf bones typically grow faster than the surrounding soft tissues, which means the Achilles tendon is pulled uncomfortably tight. At the same time, until the cartilage of the heel bone is ossified (turned into bone), it is a vulnerable spot. The tightened calf muscles cause a traction on this weak spot, resulting in pain and inflammation.
Treatment usually includes relative rest, ice, modifying activities, orthomechanical control if required to limit traction from the Achilles. Sever's disease is self- limiting and rarely causes long-term problems.


Hypermobility Syndrome



Hypermobility Syndrome
Hypermobility is a commonly used term for joints that people describe as “double-jointed”. The correct medical terminology is “A joint that has a range of motion that is beyond normal limits”. This differs from “flexibility” which is the description of normal range. It is more commonly found in females and can increase risk of injury.
Hypermobility can be a feature of other medical conditions of the thyroid and endocrine systems, as well as connective tissue disorders like Ehlers Danlos, so it is important to identify early.
Peak has experienced practitioners in the area of hypermobility, the tests needed to assess the extent of hypermobility, and then how to guide our patients through a prevention program and avoidance of the high risk of injury. Along with a network of specialists in the area to provide a collaborative approach to address all areas.
Identification of hypermobility especially in paediatrics means our ability to provide early education to both the child and family where genetics can play a big part in improving outcomes for children and adults alike.


Osgood-Schlatter Disease (OSD)



Osgood-Schlatter Disease (OSD)
Osgood–Schlatter is a painful syndrome that affects the adolescents. During a growth spurt, it is thought that the tendon attaching the quadriceps muscle to the knee joint becomes tighter, creating a strain on the growing leg bone (tibial tuberosity), particularly with physical activities that involve contraction of these muscles.
Treatment options include icing, modification of activity levels with a guided return. Stretching and strengthening of the quadriceps. Orthomechanical foot control which can certainly help with stability of the knees.
Osgood–Schlatter Syndrome will usually resolve spontaneously.


Walking & Running Concerns



Walking & Running Concerns
Does your child run funny?
Early podiatry intervention is crucial for preventing long-term issues and ensuring your child's overall foot health. From flat feet to toe-walking, our specialized pediatric podiatrists are here to evaluate and treat a wide range of gait abnormalities. By addressing these concerns early on, we can help your child develop strong, healthy feet and avoid complications later in life. Our team uses gentle, child-friendly approaches to make sure every visit is a positive experience.
Whether your little one is just starting to take their first steps or is already sprinting around the playground, our podiatry services can provide the support and care they need. We understand that each child is unique, and we tailor our treatments to fit their individual needs. So, if you notice anything unusual about your child's walking or running, don't hesitate to reach out. Let's work together to keep those tiny feet moving confidently and comfortably!
So what kinds of foot and ankle problems should parents look for?
The most common foot problem ignored in children is a flexible flat foot. This can be seen in combination with in-toeing or out-toeing as well. These kids have an arch that collapses to the ground when they bear weight or walk. Their foot is unstable and often their ankle collapses in as well when they walk. Some accommodate for this problem by out-toeing. Often, the child will actually in-toe to try to stabilise their foot.
These kids have trouble running fast and also may have trouble standing on their toes. They fatigue easily and are wearing out their shoes excessively. The problem with early diagnosis is that it is normal to have a low arched foot before the age of 3 and most children do not have a well developed arch before age 4-6 years of age.
Gait analysis and physical exam by Peak’s podiatrist can help guide parents on whether their child’s foot is normal. Most children with mild to moderate flexible flat foot can be treated gently with stretching, sturdy shoes and a pre-fabricated medical orthotic device. Some need physical therapy and a custom orthotic. Only severe flat feet require surgical correction and surgery should not be contemplated unless the child has failed the more conservative approach.
The second most commonly seen children’s foot deformity is actually the opposite of a flat foot. These children have an extremely high arched or cavus foot. Many have metatarsus adductus, which is a curving of the metatarsals or long bones in the forefoot toward the midline of the body. These kids have Cshaped feet early on and are often irritated with wearing shoes because they don’t fit right. They also may have trouble with tripping and falling. They literally trip over their own feet in gait.
A child with a cavus foot is more comfortable walking on their toes, so are often brought into the office with a complaint of toe walking. Many children with cavus feet actually have an underlying neurological problem, but it is just as common that they inherited this foot type. If this foot type is identified in the first few months of life, casting and bracing can often help correct the deformity. In an older child, physical therapy and orthotics are quite helpful.
So, why should a parent treat their child’s foot if it does not hurt?
Having excessively flexible flat feet or a rigid high arched foot causes the child to have abnormal biomechanics. What does that mean? It means they walk funny and put abnormal pressures on their other joints. The knees, hips and lower back take a beating in these foot types. Think of your feet as tyres on a car. If you have a wobbly tire or a bald spot in your tire, the struts wear out. In this case, the struts are your knees, hips and lower back.
What else can happen from abnormal feet? Common childhood foot complaints of calcaneal apophysitis known as Severs Disease (irritation of the heel growth plate), Achilles tendonitis and reoccurring sprained ankles are linked with an underlying foot deformity. If your child walks or runs funny, a life of foot and ankle pain can be avoided by a thorough assessment and guidance at Peak. Don’t assume they are going to “grow out of it.”
Visit our children specialist team at Peak Podiatry and have your child’s foot fully evaluated.


Balance and Strength



Balance and Strength
Have you noticed your child is clumsy? Your child trips over a lot or tends to be a little injury prone?
Do they prefer to sit down rather than stand and grumble if having to walk a long way?
Strength and control form a vital part of foot and lower limb function, particularly at a younger age. Lack of strength will contribute to a lack of control. When we refer to strength, it’s not about being able to lift heavy things. It’s about having strength to support your own body weight and enable moving and walking efficiency.
There are numerous tests that can be performed to assess this in children such as the Y balance test and start excursion test to name a few. A few simple exercises can greatly assist in the improvement of such areas.
This balance and strength provided the foundation for movement. Simple pointers to focus on with technique with walking and running can have profound benefits to function, performance and confidence.
Want to test your child?
Have your child stand on 1 leg , with the other leg off the ground. They may use their arms to balance.
A child up to 8 years should be able to balance for a minimum of 10 seconds.
If you have any concerns please feel free to contact our expert team or make an appointment on the link below.

General care

Blisters



Blisters
These are commonly found amongst athletes and can lead to pain and infection if left untreated. A blister occurs when a tear occurs between the top layers of the skin. The tearing occurs from repeated shearing stresses caused by frictional forces applied to the skin. The shearing is often caused from objects such as socks, an innersole, shoes or even from the ground itself.
Podiatrists not only focus on the immediate treatment of the blisters using sterile techniques, but also advise on possible preventative measures. Structural abnormalities and biomechanical dysfunction which increase shearing stresses can also be addressed.


Corns and Callus



Corns and Callus
Corns and calluses are annoying and sometimes painful thickenings in the skin in areas of repeated pressure. A corn is a small area of skin which has become thickened due to pressure on it. It can be roughly round in shape. A callus is a larger and broader area than a corn and has less well-defined edges occurring primarily on the sole of the foot.
A common cause is wearing poorly fitting shoes. A Podiatrist is qualified to diagnose and treat these conditions and can advise on footwear, shoe insoles (if required) and padding to prevent recurrences.


Warts



Warts
Often referred to as plantar warts. These can be found anywhere on the sole of the foot or the toes but tend to produce symptoms in areas of pressure and friction. The virus that causes warts, infects the superficial layer of the skin, producing a thickened callus-like growth that can become quite tender.
Although warts characteristically resolve spontaneously, they occasionally require treatment when symptomatic. Warts can either be frozen (cryotherapy), treated with powerful topical applications (chemotherapy), or can be removed surgically. The treatment of choice is made by your Podiatrist, depending on the size and area that is affected.


Cracked Heels



Cracked Heels
Dry, cracked heels can not only be unsightly, but can often cause a large amount of pain and discomfort. These are often caused by cracking or splitting of the skin. The splitting may be secondary to dryness or extreme thickening that cracks and breaks under pressure. Causes can vary from walking excessive amounts in thongs or open sandals, genetics, increased weight and long periods of standing especially on harder surfaces.
Podiatrists can treat cracked heels quickly and effectively by carefully removing the dead skin. Advice can also be provided on various cream options to use for your skin type.


Cracked Heels



Cracked Heels
Dry, cracked heels can not only be unsightly, but can often cause a large amount of pain and discomfort. These are often caused by cracking or splitting of the skin. The splitting may be secondary to dryness or extreme thickening that cracks and breaks under pressure. Causes can vary from walking excessive amounts in thongs or open sandals, genetics, increased weight and long periods of standing especially on harder surfaces.
Podiatrists can treat cracked heels quickly and effectively by carefully removing the dead skin. Advice can also be provided on various cream options to use for your skin type.

Warts



Warts
Often referred to as plantar warts. These can be found anywhere on the sole of the foot or the toes but tend to produce symptoms in areas of pressure and friction. The virus that causes warts, infects the superficial layer of the skin, producing a thickened callus-like growth that can become quite tender.
Although warts characteristically resolve spontaneously, they occasionally require treatment when symptomatic. Warts can either be frozen (cryotherapy), treated with powerful topical applications (chemotherapy), or can be removed surgically. The treatment of choice is made by your Podiatrist, depending on the size and area that is affected.

Corns and Callus



Corns and Callus
Corns and calluses are annoying and sometimes painful thickenings in the skin in areas of repeated pressure. A corn is a small area of skin which has become thickened due to pressure on it. It can be roughly round in shape. A callus is a larger and broader area than a corn and has less well-defined edges occurring primarily on the sole of the foot.
A common cause is wearing poorly fitting shoes. A Podiatrist is qualified to diagnose and treat these conditions and can advise on footwear, shoe insoles (if required) and padding to prevent recurrences.

Blisters



Blisters
These are commonly found amongst athletes and can lead to pain and infection if left untreated. A blister occurs when a tear occurs between the top layers of the skin. The tearing occurs from repeated shearing stresses caused by frictional forces applied to the skin. The shearing is often caused from objects such as socks, an innersole, shoes or even from the ground itself.
Podiatrists not only focus on the immediate treatment of the blisters using sterile techniques, but also advise on possible preventative measures. Structural abnormalities and biomechanical dysfunction which increase shearing stresses can also be addressed.

Balance and Strength



Balance and Strength
Have you noticed your child is clumsy? Your child trips over a lot or tends to be a little injury prone?
Do they prefer to sit down rather than stand and grumble if having to walk a long way?
Strength and control form a vital part of foot and lower limb function, particularly at a younger age. Lack of strength will contribute to a lack of control. When we refer to strength, it’s not about being able to lift heavy things. It’s about having strength to support your own body weight and enable moving and walking efficiency.
There are numerous tests that can be performed to assess this in children such as the Y balance test and start excursion test to name a few. A few simple exercises can greatly assist in the improvement of such areas.
This balance and strength provided the foundation for movement. Simple pointers to focus on with technique with walking and running can have profound benefits to function, performance and confidence.
Want to test your child?
Have your child stand on 1 leg , with the other leg off the ground. They may use their arms to balance.
A child up to 8 years should be able to balance for a minimum of 10 seconds.
If you have any concerns please feel free to contact our expert team or make an appointment on the link below.

Walking & Running Concerns



Walking & Running Concerns
Does your child run funny?
Early podiatry intervention is crucial for preventing long-term issues and ensuring your child's overall foot health. From flat feet to toe-walking, our specialized pediatric podiatrists are here to evaluate and treat a wide range of gait abnormalities. By addressing these concerns early on, we can help your child develop strong, healthy feet and avoid complications later in life. Our team uses gentle, child-friendly approaches to make sure every visit is a positive experience.
Whether your little one is just starting to take their first steps or is already sprinting around the playground, our podiatry services can provide the support and care they need. We understand that each child is unique, and we tailor our treatments to fit their individual needs. So, if you notice anything unusual about your child's walking or running, don't hesitate to reach out. Let's work together to keep those tiny feet moving confidently and comfortably!
So what kinds of foot and ankle problems should parents look for?
The most common foot problem ignored in children is a flexible flat foot. This can be seen in combination with in-toeing or out-toeing as well. These kids have an arch that collapses to the ground when they bear weight or walk. Their foot is unstable and often their ankle collapses in as well when they walk. Some accommodate for this problem by out-toeing. Often, the child will actually in-toe to try to stabilise their foot.
These kids have trouble running fast and also may have trouble standing on their toes. They fatigue easily and are wearing out their shoes excessively. The problem with early diagnosis is that it is normal to have a low arched foot before the age of 3 and most children do not have a well developed arch before age 4-6 years of age.
Gait analysis and physical exam by Peak’s podiatrist can help guide parents on whether their child’s foot is normal. Most children with mild to moderate flexible flat foot can be treated gently with stretching, sturdy shoes and a pre-fabricated medical orthotic device. Some need physical therapy and a custom orthotic. Only severe flat feet require surgical correction and surgery should not be contemplated unless the child has failed the more conservative approach.
The second most commonly seen children’s foot deformity is actually the opposite of a flat foot. These children have an extremely high arched or cavus foot. Many have metatarsus adductus, which is a curving of the metatarsals or long bones in the forefoot toward the midline of the body. These kids have Cshaped feet early on and are often irritated with wearing shoes because they don’t fit right. They also may have trouble with tripping and falling. They literally trip over their own feet in gait.
A child with a cavus foot is more comfortable walking on their toes, so are often brought into the office with a complaint of toe walking. Many children with cavus feet actually have an underlying neurological problem, but it is just as common that they inherited this foot type. If this foot type is identified in the first few months of life, casting and bracing can often help correct the deformity. In an older child, physical therapy and orthotics are quite helpful.
So, why should a parent treat their child’s foot if it does not hurt?
Having excessively flexible flat feet or a rigid high arched foot causes the child to have abnormal biomechanics. What does that mean? It means they walk funny and put abnormal pressures on their other joints. The knees, hips and lower back take a beating in these foot types. Think of your feet as tyres on a car. If you have a wobbly tire or a bald spot in your tire, the struts wear out. In this case, the struts are your knees, hips and lower back.
What else can happen from abnormal feet? Common childhood foot complaints of calcaneal apophysitis known as Severs Disease (irritation of the heel growth plate), Achilles tendonitis and reoccurring sprained ankles are linked with an underlying foot deformity. If your child walks or runs funny, a life of foot and ankle pain can be avoided by a thorough assessment and guidance at Peak. Don’t assume they are going to “grow out of it.”
Visit our children specialist team at Peak Podiatry and have your child’s foot fully evaluated.

Osgood-Schlatter Disease (OSD)



Osgood-Schlatter Disease (OSD)
Osgood–Schlatter is a painful syndrome that affects the adolescents. During a growth spurt, it is thought that the tendon attaching the quadriceps muscle to the knee joint becomes tighter, creating a strain on the growing leg bone (tibial tuberosity), particularly with physical activities that involve contraction of these muscles.
Treatment options include icing, modification of activity levels with a guided return. Stretching and strengthening of the quadriceps. Orthomechanical foot control which can certainly help with stability of the knees.
Osgood–Schlatter Syndrome will usually resolve spontaneously.

Hypermobility Syndrome



Hypermobility Syndrome
Hypermobility is a commonly used term for joints that people describe as “double-jointed”. The correct medical terminology is “A joint that has a range of motion that is beyond normal limits”. This differs from “flexibility” which is the description of normal range. It is more commonly found in females and can increase risk of injury.
Hypermobility can be a feature of other medical conditions of the thyroid and endocrine systems, as well as connective tissue disorders like Ehlers Danlos, so it is important to identify early.
Peak has experienced practitioners in the area of hypermobility, the tests needed to assess the extent of hypermobility, and then how to guide our patients through a prevention program and avoidance of the high risk of injury. Along with a network of specialists in the area to provide a collaborative approach to address all areas.
Identification of hypermobility especially in paediatrics means our ability to provide early education to both the child and family where genetics can play a big part in improving outcomes for children and adults alike.

Sever's Disease



Sever's Disease
Looking at a child limping off the ground and complaining about pain in their heels is never pleasant.
Sever's disease is the most common cause of heel pain particularly in the young and physically active child. Just before puberty the calf bones typically grow faster than the surrounding soft tissues, which means the Achilles tendon is pulled uncomfortably tight. At the same time, until the cartilage of the heel bone is ossified (turned into bone), it is a vulnerable spot. The tightened calf muscles cause a traction on this weak spot, resulting in pain and inflammation.
Treatment usually includes relative rest, ice, modifying activities, orthomechanical control if required to limit traction from the Achilles. Sever's disease is self- limiting and rarely causes long-term problems.

Knee Arthritis



Knee Arthritis
Osteoarthritis (OA) is the most common form of knee arthritis which is a degenerative joint disease that can gradually wear down the cartilage in the joint. This results in severe pain and stiffness in the joint. OA can affect both sides of the knee but the most common side affected is the inner (medial) side. Common causes of knee arthritis can range from previous trauma to the area, poor biomechanics of the feet, obesity and genetics.
Treatments often revolve around reducing the impact aggravating the condition. Strengthening exercises are often advised but customised orthotics have been shown to help reduce symptoms.

Knee Pain



Knee Pain
Knee pain is a common problem with many causes, ranging from acute injuries, various medical conditions and overuse. It can be localised to a specific area of the knee or be diffuse throughout the knee. Most knee conditions are often accompanied by physical restriction and a thorough physical examination will usually establish the diagnosis.
Common types of knee pain seen by Podiatrists include:
- Patellofemoral pain
- Iliotibial Band Friction Syndrome
- Ligament injuries
- Osteoarthritis
Podiatrists are primary health care providers of the feet and lower limb and commonly treat conditions like these.

Patellafemoral



Patellafemoral
This refers to pain arising from under and around the kneecap. The kneecap is designed to move up and down within a special groove at the end of the thigh bone. If the kneecap starts to track to the side (misaligned), pain develops.
With this repeated movement the cartilage behind the kneecap can also become irritated. The most common symptom experienced is pain worsening with running and also going up and down stairs. Common causes can be poor foot mechanics, improper footwear and weakness or an imbalance of the quadriceps muscles.
Treatment will include an adequate gait assessment and review of shoes. Together with strengthening of the affected musculatures, orthotic therapy is often needed to improve foot biomechanics and is effective in resolving pain.

Foot & Leg Cramps



Foot & Leg Cramps
A muscle cramp is a strong, painful contraction or tightening of a muscle that typically comes on suddenly and can last anywhere from a few seconds to several minutes. It often occurs in the legs and through the calf muscles. However, sometimes it occurs in the small intrinsic foot muscles and is misdiagnosed.
Specific stretching, taping, dry needling and massage techniques can make a massive difference and rid you of any symptoms. Sometimes the cramps are secondary to poor lower limb biomechanics and that can be augmented with footwear modifications or orthotic therapy.

Calf Strain



Calf Strain
This is a condition caused by a tear of the muscle fibres of the muscles at the back of the lower leg and can range from mild to very severe. Calf injuries usually occur as a result of a sudden pushing off movement or from excessive over-stretching of the calf muscles as demonstrated in jumping activities or during quick changes of direction.
Treatment can include rest, ice, and compression in the acute stages followed by a full rehabilitation programme of strength and stretching exercises. Often Podiatrists will analyse a person’s gait and footwear to ascertain if control is adequate to also prevent further injury.

Shin Pain



Shin Pain
This is a common injury in many running based sports. It is characterised by pain in and around the tibia (shin bone) in the lower leg and usually occurs as a result of a sudden increase in the frequency, duration and/or intensity of activity.
People at risk are those with abnormal biomechanics, using inappropriate footwear for the activity and often poor flexibility. Prevention initially starts with undertaking adequate and supervised training.
Programmes may be required to develop strength, balance, coordination and flexibility. Wearing the appropriate footwear for your foot type and considering a biomechanical foot screening to determine if further orthomechanical control is required.
Like most overuse injuries, shin pain may develop gradually over a period of time but if assessed and treated early, a return to normal activity levels can be easily achieved.

Forefoot Pain



Forefoot Pain
The forefoot (or ball of the foot) is made up of small bones, muscles, ligaments, tendons and many other forms of soft tissues. This makes pain in this area complex to diagnose. An expert knowledge of the anatomy of the forefoot allows an in-depth examination and the injured structure can be easily identified. Often the diagnosis can be as diverse a painful corn or callus to an entrapped nerve.
Management is directed towards targeting the cause and condition, and measures put in place to offload the affected area. These may include a change of footwear or modifications and possibly shoes orthoses. Massage and other forms of remedial therapy can always help.

Bunions and Big Toe Joint Pain



Bunions and Big Toe Joint Pain
Are you starting to notice a lump or bump on the side of your big toe?
Are you experiencing pain in this joint when you are wearing shoes?
Bunions are extremely common conditions seen by Podiatrists. They are often seen as a bony lump near the base of the big toe joint which can eventually lead to osteoarthritis. The first toe joint plays an extremely important role in how we function during walking and running, and changes to this joint can reflect further than the foot itself.
A conservative approach is usually the first line of treatment, all depending on the individual and stage of the deformity. Re-aligning the foot with the aid of an orthotic can prevent further degeneration. Along with this, a change of footwear may help decrease the pressure and compliment the orthotics. Surgical correction of the bunion is another option but should only be considered if the conservative measures have failed.

Cuboid Syndrome



Cuboid Syndrome
Do you have lateral foot pain (outer side of your foot) that either aches or feels like the pain moves around? Sometimes even feels slightly locked up?
The Cuboid is an important bone in the lateral arch of the foot that can subtly ‘sublux’ when enough force is applied by a tendon that travels over it called the Peroneus Longus This can occur as a one off “incident”, like a slight sprain of the ankle, or gradual tightening of the Peroneus Longus caused by overuse.
While cuboid syndrome is relatively common it is hard to identify so is commonly misdiagnosed. It is important to get it treated early so as to “reposition” the cuboid back into its original place. There can be long term effects on the calcaneocuboid joint and surrounding structures if left in a ‘subluxed’ position for too long.
Biomechanics can play a large part in the foot type that sustains this injury so it is important to always have it assessed by a Podiatrist.

Rolled Ankles



Rolled Ankles
This is a very common injury occurring during a wide variety of sports and activities. Usually the ankle “rolls-in” and ligaments and tendons on the outside become aggravated, damaged and sometimes torn depending on the severity of the injury.
The most commonly injured structure is the Anterior Talofibular Ligament (ATFL), which connects the talus to the fibula on the outside of the ankle. It is important to rest, ice, apply compression and elevate the ankle immediately and up-to 48 hours after injury to help with swelling.
If pain persists 48 hours after injury it is always a good idea to see one of our Podiatrists to assess the extent of injury. This is critical as the most important aspect of any ankle injury is setting-up an appropriate rest and rehab protocol. The chances of rolling the same ankle again are significantly higher without appropriate rest and rehab.

Metatarsal Stress Fractures



Metatarsal Stress Fractures
Stress fractures refer to a tiny “crack” in a bone caused by repetitive stress or force, often from overuse. Approximately 10% of all stress fractures are localised to the metatarsal bones of the foot. Football, basketball, gymnastics, ballet and running are often associated with metatarsal stress fractures.
Symptoms include Insidious onset of pain, frequently worsened with activity with no recollection of trauma or trauma which is 1-2 week(s) prior symptoms. Although x-rays are often utilised in the diagnosis of stress fractures, clinical examinations alone are usually reliable in making the diagnosis.
Footwear modification, activity modification, carbon plates and/or specialised boots are all examples of the immediate treatment available. In the long-term, we can also provide biomechanical assessments to determine if an underlying biomechanical dysfunction is predisposing to the stress fracture and prevent reoccurrence.

Morton's Neuroma



Morton's Neuroma
Are you experiencing a dull ache in your forefoot that sometimes turns into a sharp radiating pain into your toes? Or do you get unexplained numbness at the end of a toe/toes?
These are common symptoms that occur in a condition called Morton’s neuroma. The Morton’s Neuroma is simply described as a thickening of the nerve or surrounding tissue as it passes through the space between the Metatarsal heads. It is usually found between the 3rd and 4th metatarsals but it can occur between the others.
Compression of the forefoot from wearing shoes that are too tight is a common cause. However, there are other biomechanical causes of the pathology that always need to be assessed. In severe cases surgery may be required.

Ankle Pain



Ankle Pain
Are you getting ankle pain? You may have an obvious reason for this, like a recent sprain! However sometimes there is a not so obvious reason.
Either way it is important to have it checked out by a qualified Sports Podiatrist. The ankle is an important weight bearing joint. It can be affected by arthritis, ligament injury, fractures and various other pathologies. A thorough assessment is essential for a correct diagnosis so that the right treatment choice can be provided for you.
We aim to give you the best professional advice and care possible here at Peak Podiatry.

Flat Feet



Flat Feet
Have you ever been told, or have you always been aware that your feet are flat?
Flat feet are the postural deformity in which the arches of the foot collapse, with the entire sole of the foot coming into complete or near-complete contact with the ground. In many cases these may be asymptomatic, but flat feet are often an indication that the architecture and integrity is not correct. Your feet support the whole body, and having strong arches is important to your body’s health. With a fallen arch, your tendons and ligaments weaken and can cause pain throughout your feet, ankles, lower legs and even further up through to your hips and lower back.
Treatment will often revolve around creating stability. This can be done wearing comfortable and supportive footwear. Wearing the appropriate orthotics can also help distribute and minimise pressure in the foot by providing the additional arch support. Strength and stabilising exercises can also be incorporated for extra control.
It's also important to know that not all flat feet need support. We are here to make sure that options are discussed and expert opinion is provided where treatment IS NOT required where assistance may help. Not all flat feet need orthoses.

Plantar Fasciitis



Plantar Fasciitis
This is the most common cause of all heel pains. The plantar fascia is a band of fibrous connective tissue that runs along the sole from the heel to the ball of the foot. Bruising or over stretching this can cause inflammation particularly more towards the heel but can affect any part of the band.
It is commonly associated with long periods of weight bearing or sudden changes in activity levels Prevention and treatment will often revolve around stretching, massage, change of footwear and possibly orthotics if there is an underlying biomechanical cause.
Diabetes
At PEAK, we recognize the critical connection between diabetes and foot health. Our specialized diabetes care focuses on preventing and managing diabetic foot complications through comprehensive assessments, personalized treatment plans, and ongoing education. From routine foot health care to thorough neurovascular assessments, custom deflective and offloading orthoses and diabetic footwear, we offer the expertise and support you need to maintain healthy feet and avoid serious complications. Trust our dedicated team to help you navigate the unique challenges of diabetes and keep your feet in optimal condition. Contact us today to learn more about our personalised diabetes-focused podiatry services and take the first step towards lasting foot health.
Our Commitment to Exceptional Care
The focus at Peak Podiatry is on sports and family podiatry. We aim to provide fast effective relief to all age groups, from the very young to the elderly, with any nature of concern.
Whether you are an athlete, play occasional sports or wishing just to get back to being able to function each day pain free, our Podiatrists tend to each case with the same commitment and care.
Our commitment is to provide the highest quality podiatric treatment and education consistently and cost effectively.
At Peak Podiatry, we’re redefining podiatry with:

Holistic Care
Addressing the underlying causes of your issues, not just the symptoms.

Advanced Techniques
Leveraging the latest technology for precise diagnosis and effective treatment.

Collaborative Approach
Working with you—and your other healthcare providers if needed—for a comprehensive solution.

Patient Empowerment
We educate you every step of the way, so you feel confident in managing your health.
Your Path to Health Starts Here
We’re dedicated to helping you get back on your feet—literally and figuratively.
Let us help you move better, feel better, and live better with expert, compassionate care that truly makes a difference.
